What is MOHS Surgery?
Mohs surgery is an effective procedure for the removal of specific skin cancers. The procedure was developed in the early 20th century at the University of Wisconsin School of medicine and is now practiced throughout the United States. The procedure is different from other skin cancer treatments in that it uses an examination of the removed cancerous tissue, so that all and extensions of the cancer can be removed. Due to the tissue being removed and examined, Mohs surgery has been the highest reported cure for cancer. Doctors performing this surgery have specialized skills in dermatology, dermatologic surgery, dermatopathology, or Mohs surgery.

Basic and advanced training in Mohs surgery is taught at specific residency programs and fellowships. Also the Mohs surgeon has the required laboratory facilities on location. Your Mohs surgeon can provide you with detailed information regarding his or her training in the above disciplines, as well as all applicable professional affiliations.
It is important to note that Mohs surgery is not effective for the treatment of all skin cancers. Mohs micrographic surgery typically is reserved for those cancers that have recurred or have a high risk for recurrence. Mohs surgery also is indicated for cancers located in areas such as the nose, ears, eyelids, lips, hairline, hands, feet, and genitals, in which maximal preservation of healthy tissue is critical for cosmetic or functional purposes.
How is Mohs Surgery Done?
There are three steps involved in Mohs surgery:
1. The skin is made completely numb using a local anesthetic. The visible cancer is removed with a thin layer of additional tissue. This takes only a few minutes and the patient may then return to the waiting room. A detailed diagram (a Mohs map) of the removed specimen is then drawn.
2. The skin is color coded to distinguish top from bottom and left from right. A lab technician freezes the tissue and removed very thin slices from the entire edge and under the surface. The slices are placed on a film slide and colored for examination. This lab work may take up to an hour.
3. Your doctor then will carefully examine these slides under a microscope. The examiner will look for more signs of cancerous tissue. The entire undersurface and the complete edge of the specimen is examined.
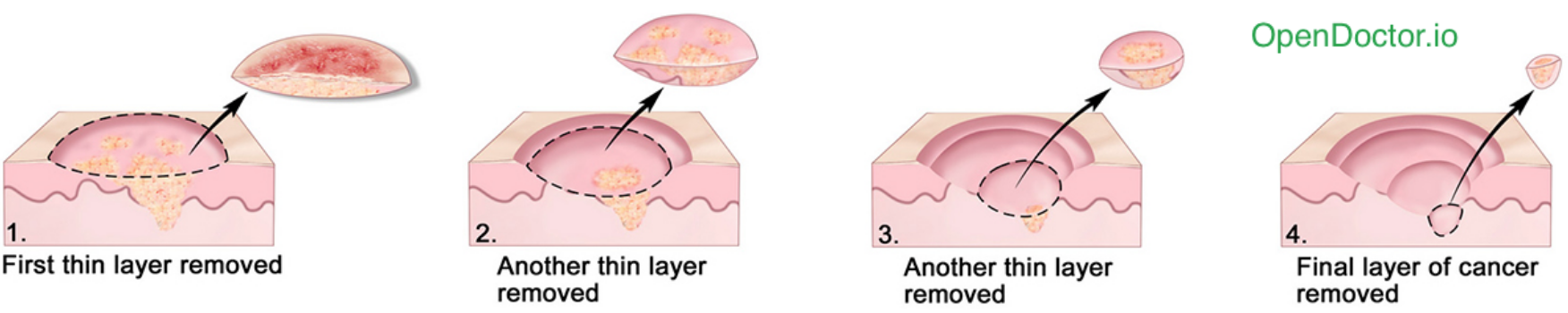
If more cancer is found on the microscopic slides, your doctor uses the Mohs map to remove additional tissue only where cancer is present. This allows the Mohs surgery technique to leave the smallest possible scar as during each stage cancer is immediately looked for. Only tissue around the "roots" and extensions of cancer is removed.
How long does it take?
Usually less than one hour. This can depend on lab work. Most cases can be completed in three of fewer stages, requiring less than four hours. However, no one can predict how extensive a cancer will be because the size of a skin cancer's "roots" cannot be estimated in advance. We therefore ask that you reserve the entire day for surgery, in case additional surgical sessions are required.
Will it leave a scar?
Yes. Any form of surgery will leave a scar. Mohs surgery; however, will leave one of the smallest possible surgical defects, and therefore a smaller final scar.
What happens after the surgery is completed?
When the cancer is removed, your doctor will discuss with you your options. These may include: 1. allowing the wound to heal naturally, without additional surgery (often produces the best cosmetic result), 2. wound repair by your doctor, 3. wound repair by the referring physician or making arrangements for wound repair, or 4. referral to another surgeon for wound closure.
How do I prepare?
Get plenty of sleep and eat normally before Mohs Surgery. If you are taking prescriptions, continue to take them unless otherwise told by your doctor. Avoid taking medications that contain aspirin for ten days before your surgery. Do not take any aspirin substitutes such as Advil, Motrin, Nalfon, Naprosyn within 24 hours of your surgery. Tylenol is acceptable at any time before the surgery. Patients often read during surgery. Do not attempt to drive yourself home.
Will I have pain after surgery?
Most patients do not complain of significant pain. If there is discomfort, Tylenol or Vicodin is usually all that is needed for relief. Sometimes, more significant pain medications will be prescribed when needed. Bruising and swelling around the wound is common.
Does insurance usually cover the cost?
Yes. Insurance policies cover the costs of Mohs surgery and the surgical reconstruction of the wound. Please check with your insurance carrier for exact information relating to your surgery - your doctor most likely accepts Medicare.